Sinus Rhythms
Sinus rhythms have five common variations.
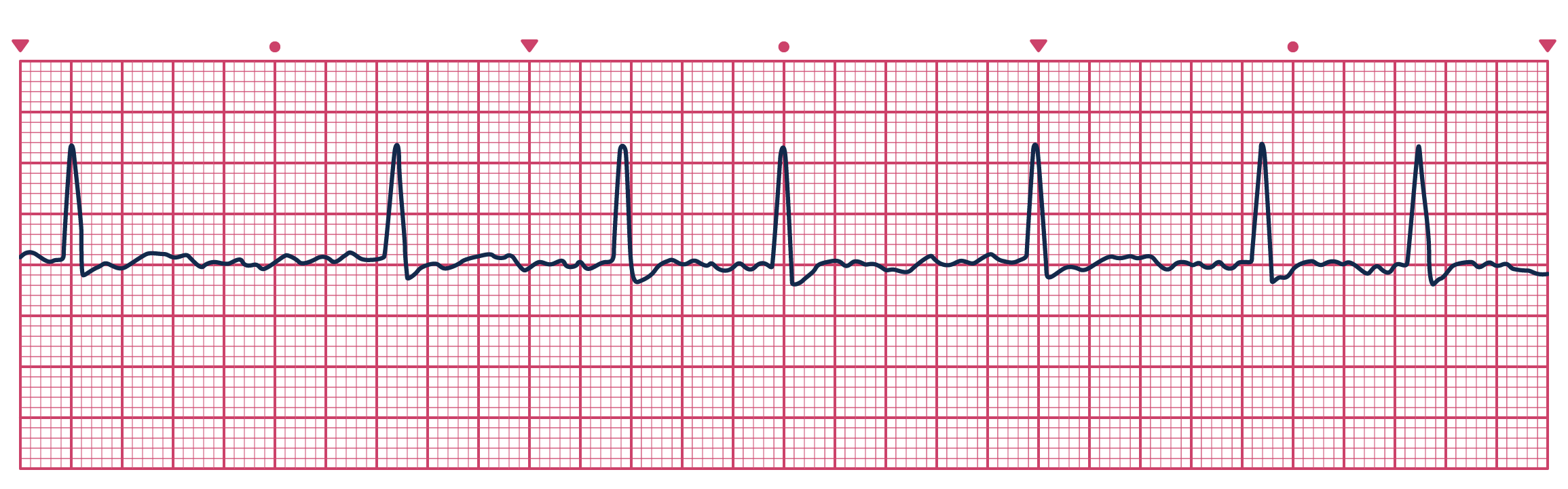
Normal Sinus Rhythm (60–100 bpm)
Sinus Bradycardia (< 60 bpm)
Treatment: Symptomatic bradycardia - atropine or pacing.
Sinus Tachycardia (> 100 bpm)
Treatment: Tachycardia with narrow QRS complexes - consider vagal maneuvers, adenosine, beta blocker (metoprolol), calcium channel blocker (diltiazem), or synchronized cardioversion. Tachycardia with wide QRS complexes - consider anti-arrhythmics, such as procainamide, amiodarone, or sotalol.
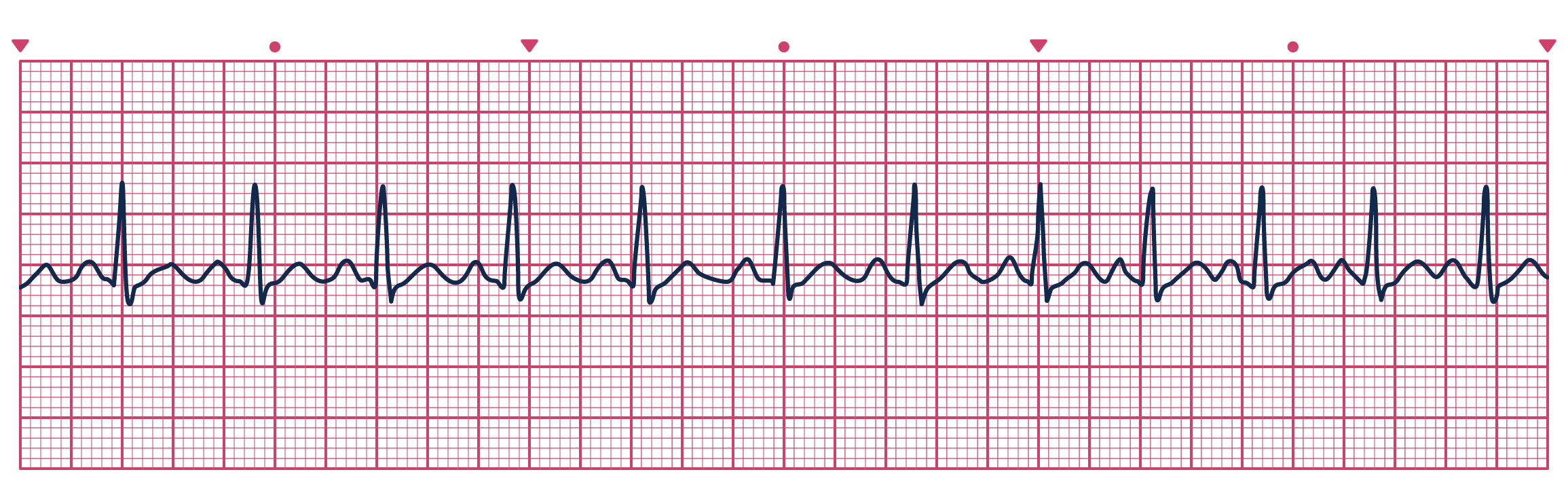
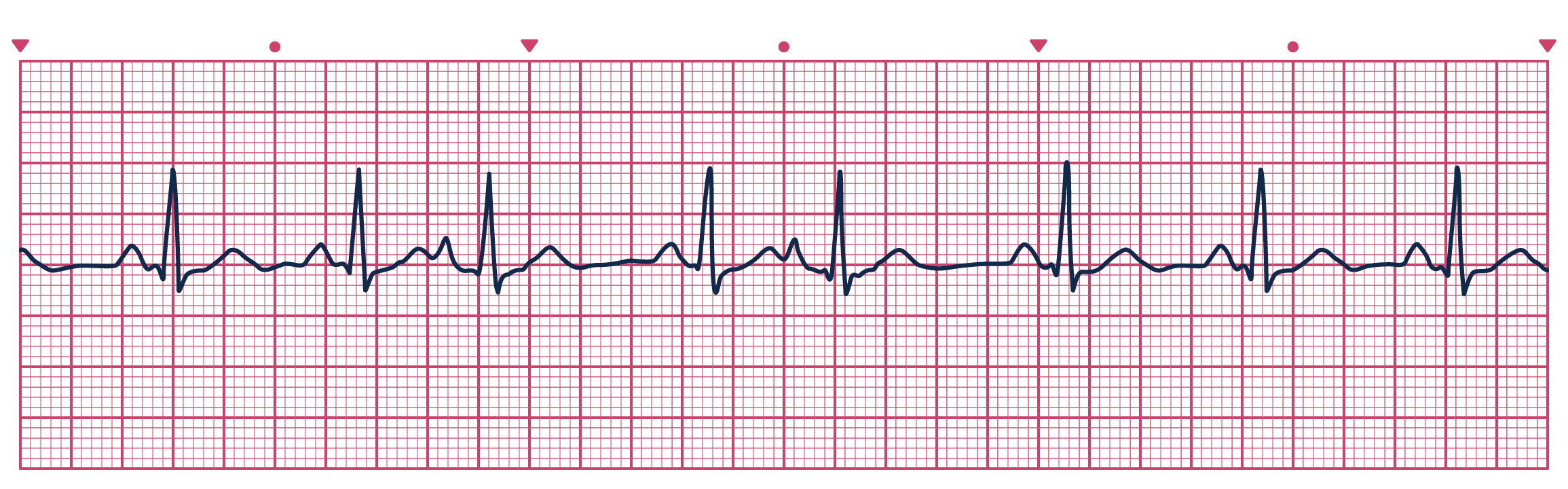
Sinus Arrhythmia (60–100 bpm)
Treatment: Sinus arrhythmia typically is asymptomatic and does not require treatment but may be reduced by avoiding caffeine and other stimulants.
Five steps to identify this heart rhythm:
- What is the rate? 60-100 beats per minute
- What is the rhythm? Irregular (varies more than 0.08 sec)
- Is there a P wave before each QRS? Are P waves upright and uniform? Yes; Yes
- What is the length of the PR interval? 0.12-0.20 seconds (3-5 small squares)
- Do all QRS complexes look alike? What is the length of the QRS complexes? Yes; 0.06-0.12 seconds (1½ to 3 small squares)
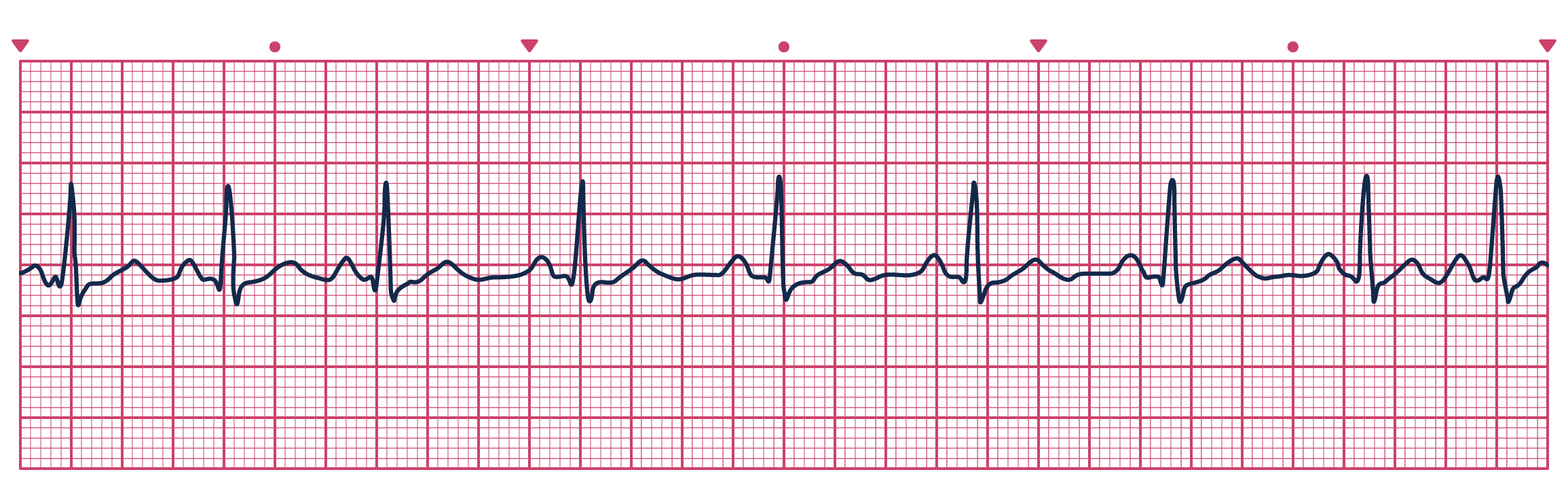
Sinus Pause
Atrial Rhythms
Atrial rhythms occur when the sinoatrial (SA) node fails to generate an impulse. Atrial tissues or internodal pathways may initiate an impulse instead. The four most common atrial arrhythmias are described here.
Atrial Flutter (rate varies; usually regular; saw-toothed)
Treatment: Cardioversion = treatment of choice; antiarrhythmics (procainamide) to convert the flutter; diltiazem, verapamil, digitalis, or a beta blocker (metroprolol) to slow the ventricular rate; heparin to reduce incidence of thrombus formation.
Five steps to identify this heart rhythm:
- What is the rate? Atrial: 250-400 bpm; ventricular: variable
- What is the rhythm? Atrial: regular; ventricular: may be irregular
- Is there a P wave before each QRS? Are P waves upright and uniform? Normal P waves are absent; flutter waves (f waves) (sawtooth pattern) are present
- What is the length of the PR interval? Not measurable
- Do all QRS complexes look alike? What is the length of the QRS complexes? Yes; 0.06-0.12 seconds (1½ to 3 small squares)
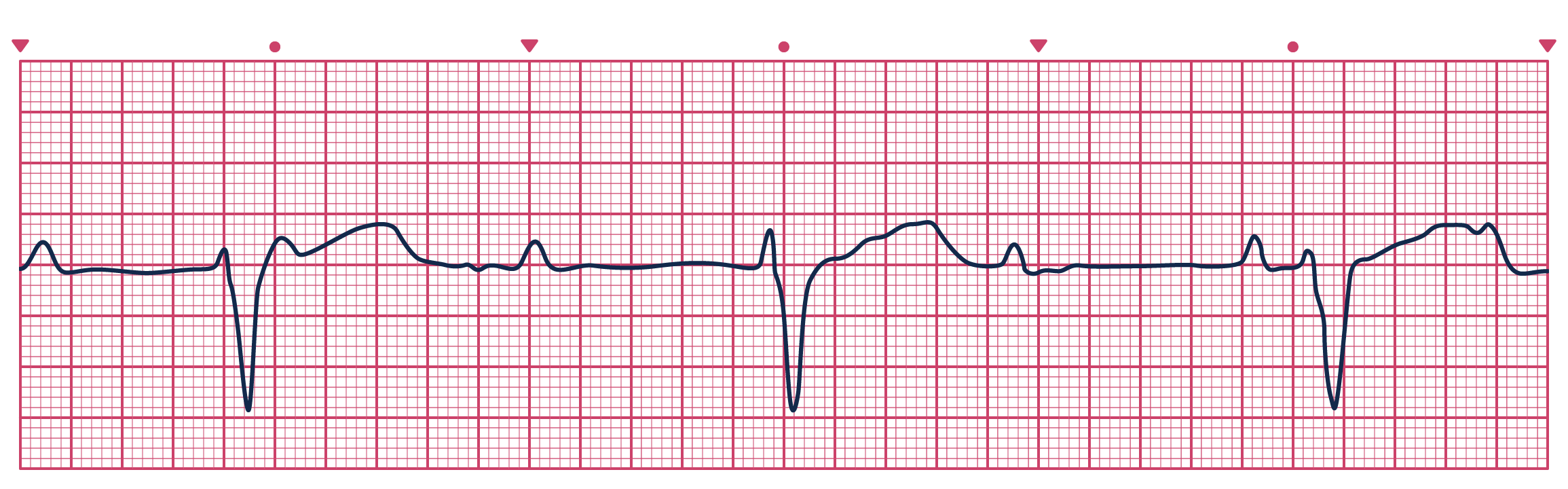
Atrial Fibrillation (rate varies; always irregular)
Treatment: Rate control (slow ventricular rate to 80-100 beats/minute) with digoxin, beta-adrenergic blockers, or calcium channel blockers (diltiazem)
Five steps to identify this heart rhythm:
- What is the rate? Atrial: 350-400 bpm; ventricular: variable
- What is the rhythm? Irregularly irregular
- Is there a P wave before each QRS? Are P waves upright and uniform? Normal P waves are absent
- What is the length of the PR interval? Not discernable
- Do all QRS complexes look alike? What is the length of the QRS complexes? Yes; 0.06-0.12 seconds (1½ to 3 small squares)
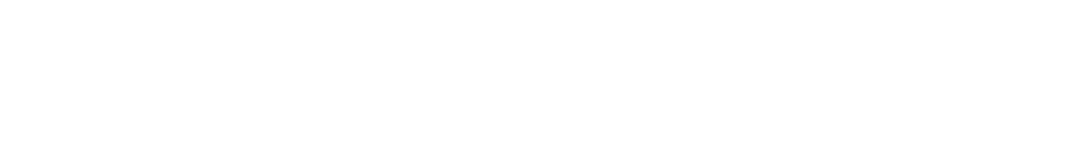
Supraventricular Tachycardia (> 150 bpm, regular rhythm)
Treatment: Vagal maneuvers or adenosine if stable; electrical cardioversion if unstable.
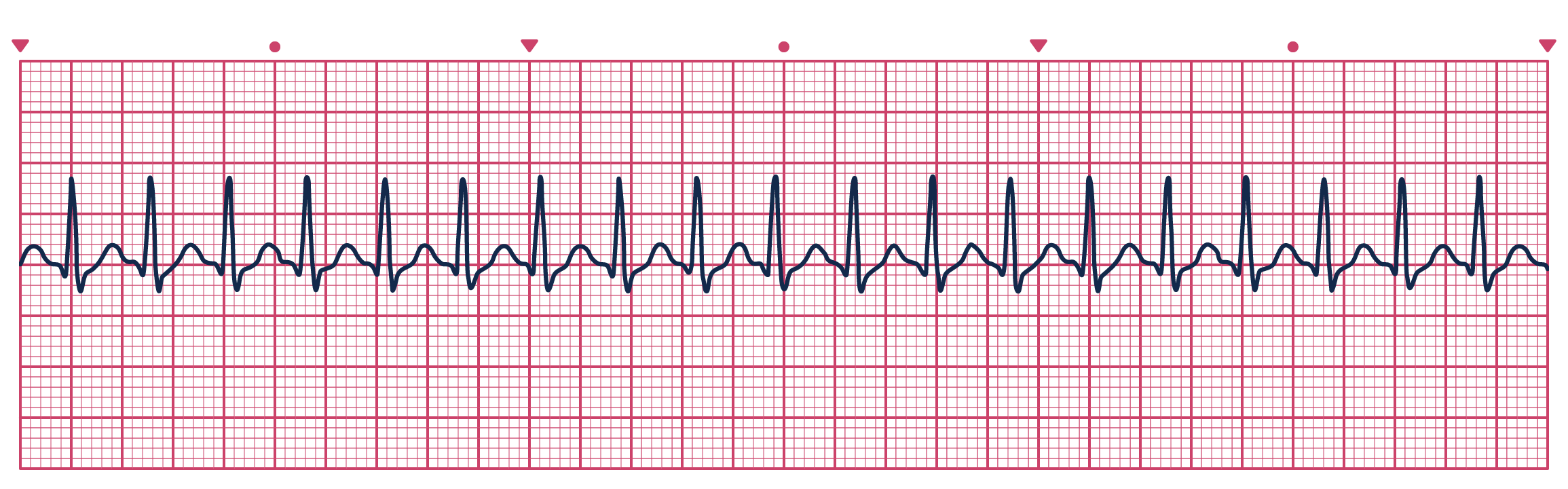
Five steps to identify this heart rhythm:
- What is the rate? Atrial: 150-250 bpm; ventricular: 150-250 bpm
- What is the rhythm? Regular
- Is there a P wave before each QRS? Are P waves upright and uniform? Usually not discernable, especially at the high rates (becomes hidden in the QRS)
- What is the length of the PR interval? Usually not discernable
- Do all QRS complexes look alike? What is the length of the QRS complexes? Yes; 0.06-0.12 seconds (1½ to 3 small squares)
Premature Atrial Complexes (PACs) (rate varies; irregular rhythm)
Treatment: None required if asymptomatic. Most people occasionally have PACs. They can worsen under stress. If symptomatic, look for underlying causes and reduce heart rate if elevated.
Five steps to identify this heart rhythm:
- What is the rate? Usually regular, but depends on the underlying rhythm
- What is the rhythm? Irregular as a result of the PAC
- Is there a P wave before each QRS? Are P waves upright and uniform? Usually upright, but premature and abnormal shape
- What is the length of the PR interval? 0.12-0.20 seconds (3-5 small boxes)
- Do all QRS complexes look alike? What is the length of the QRS complexes? Yes; 0.06-0.12 seconds (1½ to 3 small squares)
Ventricular Rhythms
When the SA node and the AV junctional tissues fail to generate an impulse, the ventricles assume the role of pacing the heart. P waves are absent because there is no atrial activity or depolarization. Ventricular rhythms display QRS complexes that are wide (greater than or equal to 0.12 seconds) and abnormal in appearance.
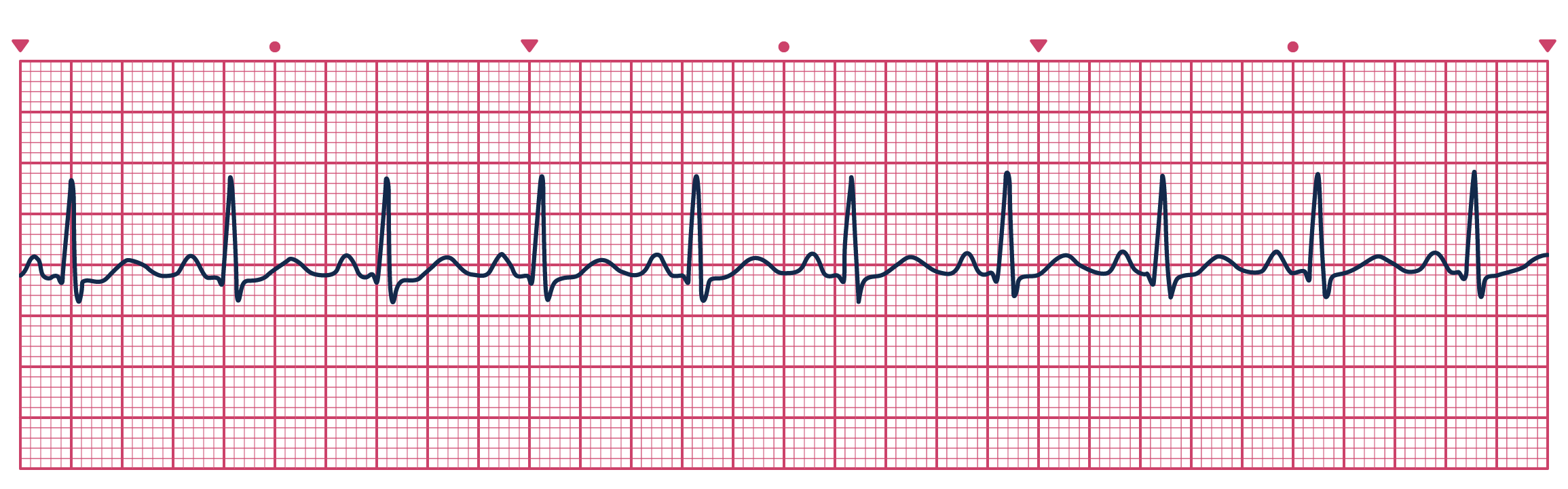
Premature Ventricular Contractions
Premature ventricular contractions (PVCs) are ectopic extra beats. PVCs are the most common ventricular dysrhythmia. Many people have these occasionally, and they don't require treatment in an otherwise healthy heart. Stress and the use of stimulants make these worse. If PVCs begin to occur more frequently (> 20-40% of all beats), they may progress to the more dangerous rhythms described later.
Treatment: Address underlying causes if possible. Lidocaine is the drug of choice.
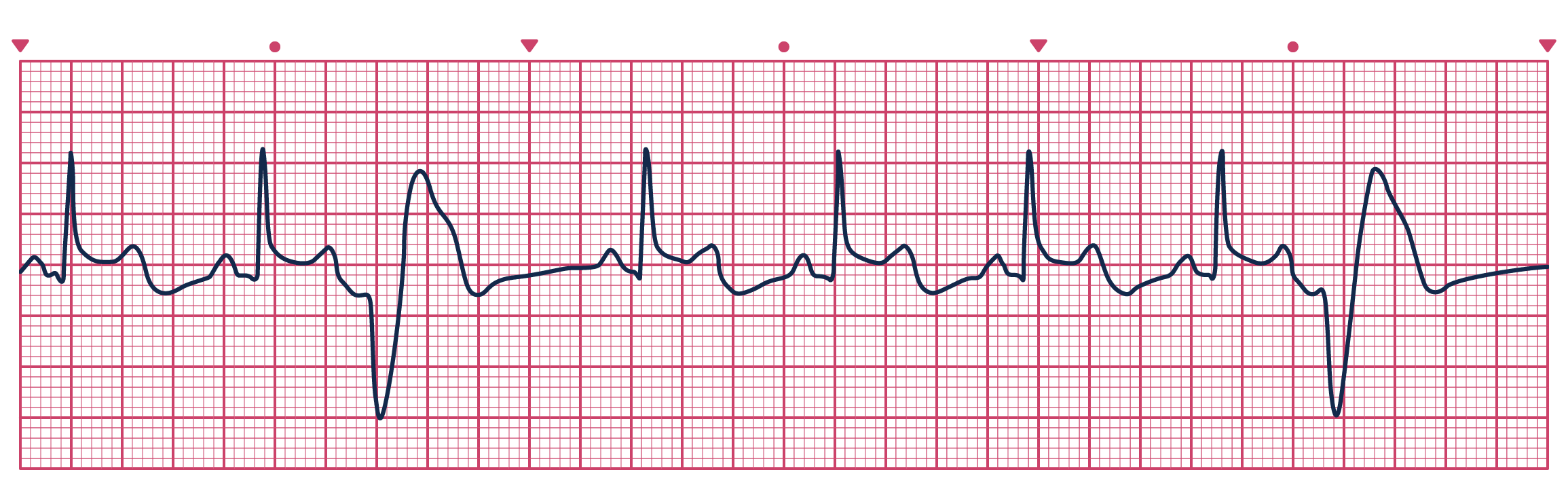
Five steps to identify this heart rhythm:
- What is the rate? Atrial: usually normal; ventricular: usually normal, depends on underlying rhythm
- What is the rhythm? Depends on underlying rhythm; irregular during PVCs
- Is there a P wave before each QRS? Are P waves upright and uniform? Absent with PVCs
- What is the length of the PR interval? Not measureable during PVCs
- Do all QRS complexes look alike? What is the length of the QRS complexes? Varies; wide and distorted (> 0.12 sec), occurs earlier than expected
Ventricular Tachycardia (> 150 bpm)
Rhythm in which three or more PVCs arise in sequence at a rate greater than 100 beats per minute. V-tach can occur in short bursts lasting less than 30 seconds, causing few or no symptoms. Sustained v-tach lasts for more than 30 seconds and requires immediate treatment to prevent death. V-tach can quickly deteriorate into ventricular fibrillation.
Treatment: If there is a pulse and the patient is unstable, cardiovert and begin amiodarone or lidocaine. If there is no pulse, begin CPR and follow ACLS protocol.
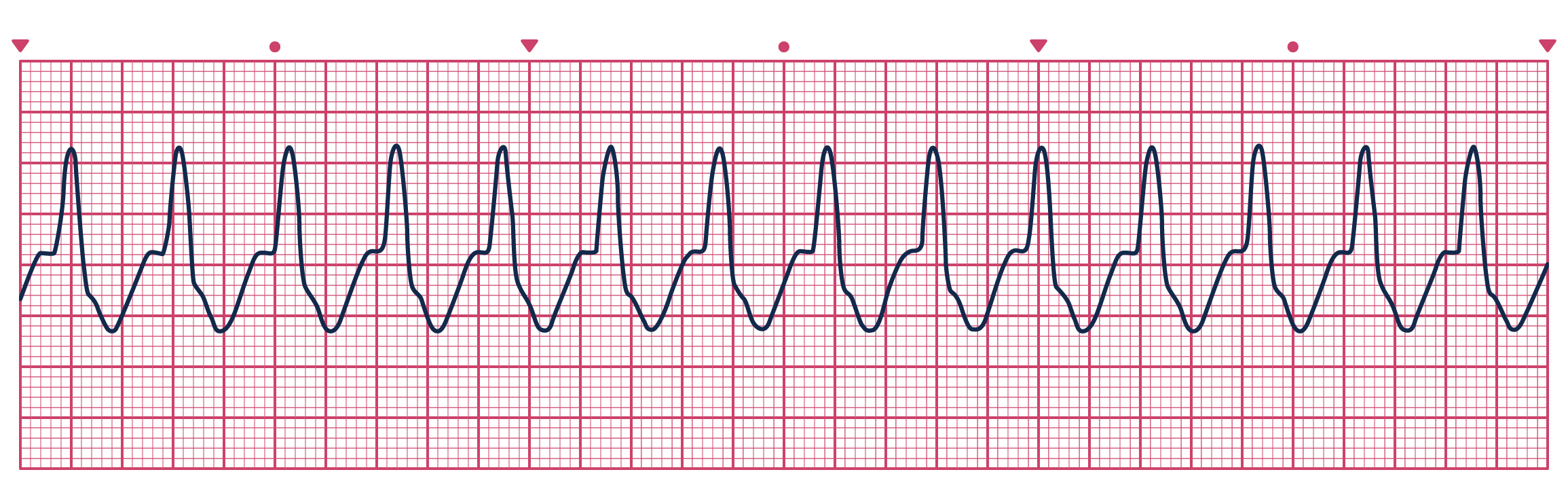
Five steps to identify this heart rhythm:
- What is the rate? 101-250 bpm
- What is the rhythm? Atrial rhythm not distinguishable; ventricular rhythm usually regular
- Is there a P wave before each QRS? Are P waves upright and uniform? No
- What is the length of the PR interval? Not measureable
- Do all QRS complexes look alike? What is the length of the QRS complexes? Wide and distorted (> 0.12 sec)
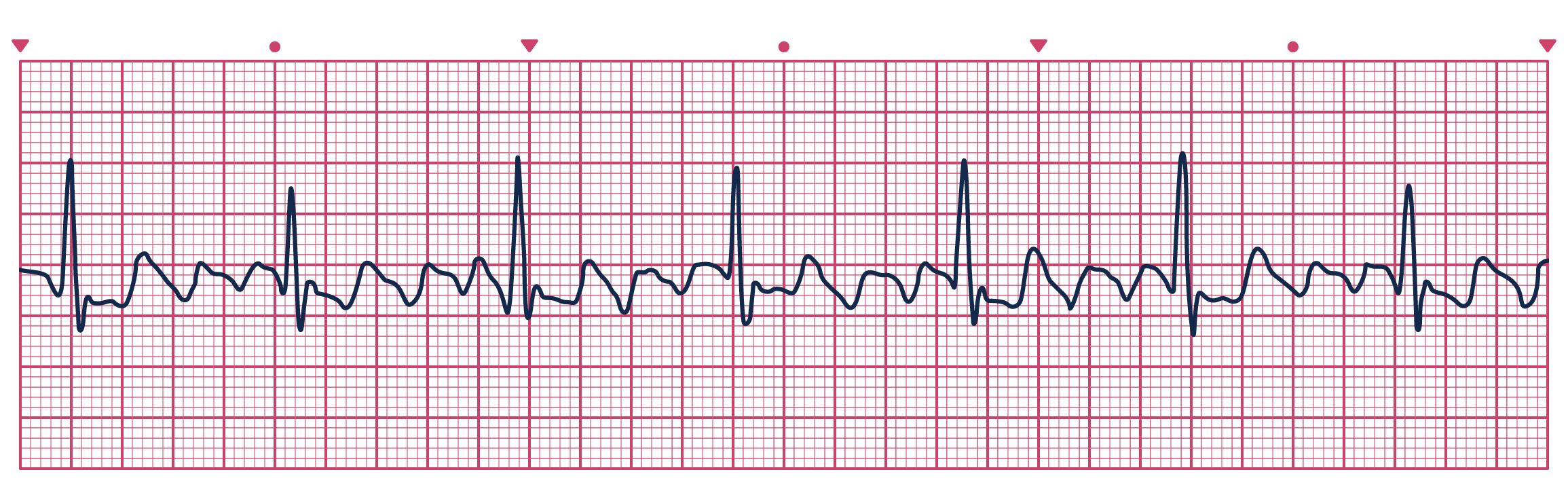
Torsades de Pointes
Associated with a prolonged QT interval. Torsades appears in short bursts that terminate spontaneously but frequently recur and degenerate into ventricular fibrillation. The hallmark of this rhythm is the upward and downward deflection of the QRS complexes around the baseline. The term 'Torsades de Pointes' means 'twisting about the points.'
Treatment: Begin CPR and ACLS measures. Administer magnesium bolus.
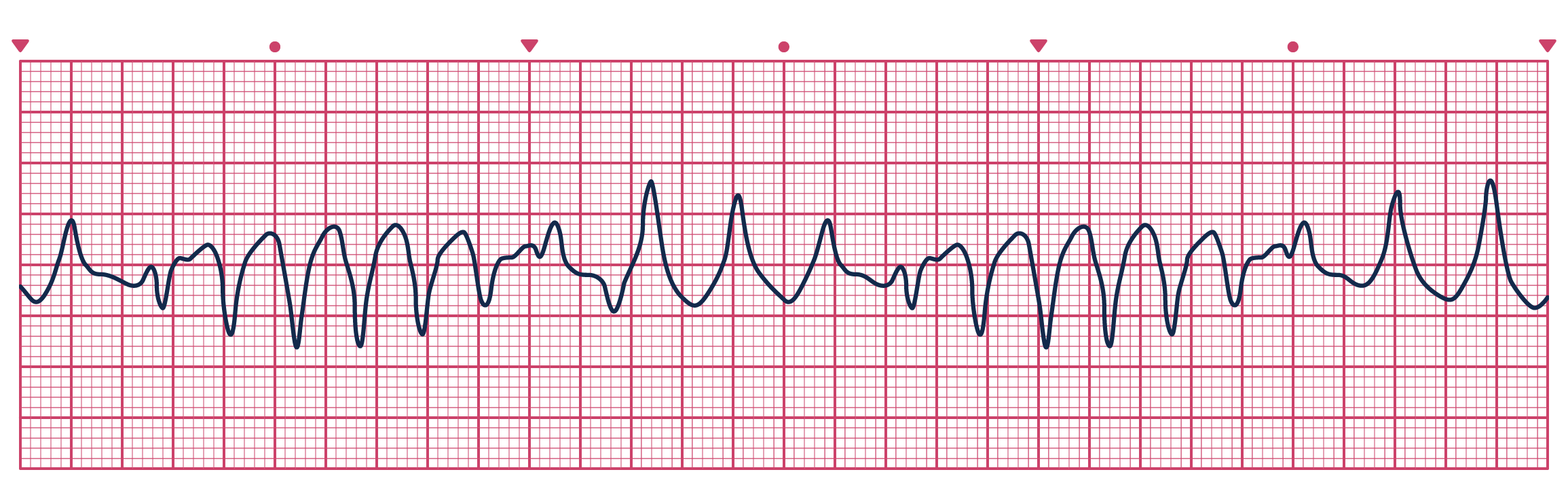
Five steps to identify this heart rhythm:
- What is the rate? Ventricular: 150-250 bpm
- What is the rhythm? Regular or irregular
- Is there a P wave before each QRS? Are P waves upright and uniform? No
- What is the length of the PR interval? Not measurable
- Do all QRS complexes look alike? What is the length of the QRS complexes? Wide and bizarre, some deflecting downward and some deflecting upward
Ventricular Fibrillation
Occurs as a result of multiple weak ectopic foci in the ventricles. Coordinated atrial or ventricular contraction is absent. Electrical impulses are initiated by multiple ventricular sites; impulses are not transmitted through normal conduction pathways. There are two types of waves: coarse (early, waves are larger and more variable) and fine (later, waves get smaller as the situation worsens).
Treatment: Administer CPR and defibrillation, and then initiate the ACLS algorithm.
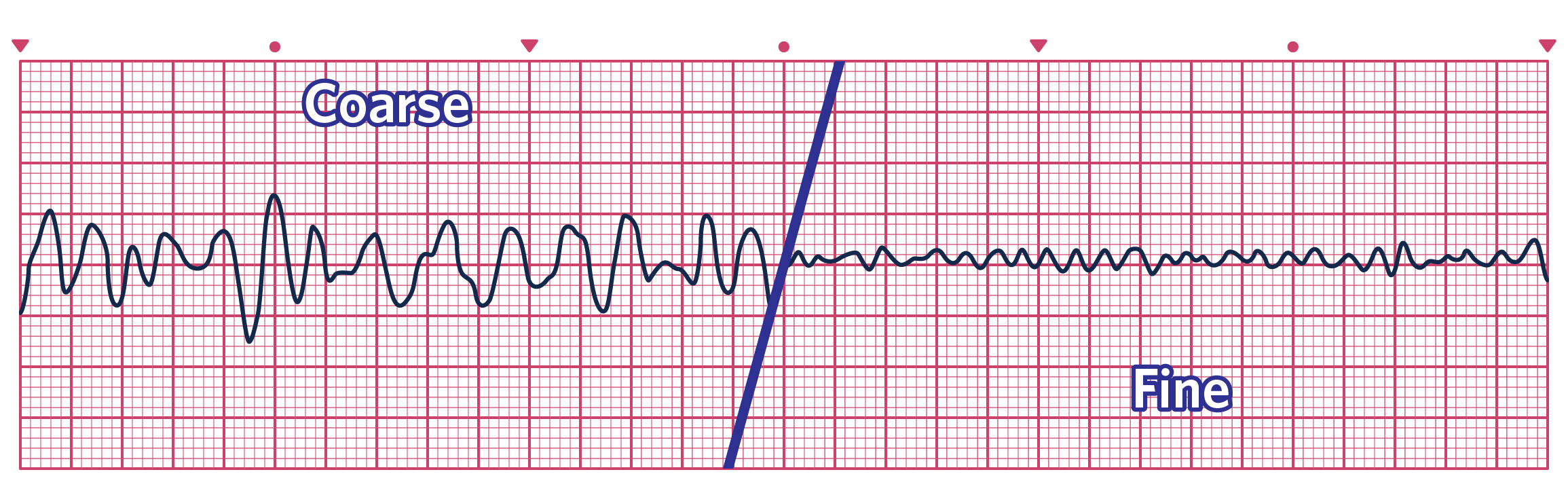
Five steps to identify this heart rhythm:
- What is the rate? Not discernible
- What is the rhythm? Rapid, unorganized, not discernible
- Is there a P wave before each QRS? Are P waves upright and uniform? No
- What is the length of the PR interval? None
- Do all QRS complexes look alike? What is the length of the QRS complexes? None
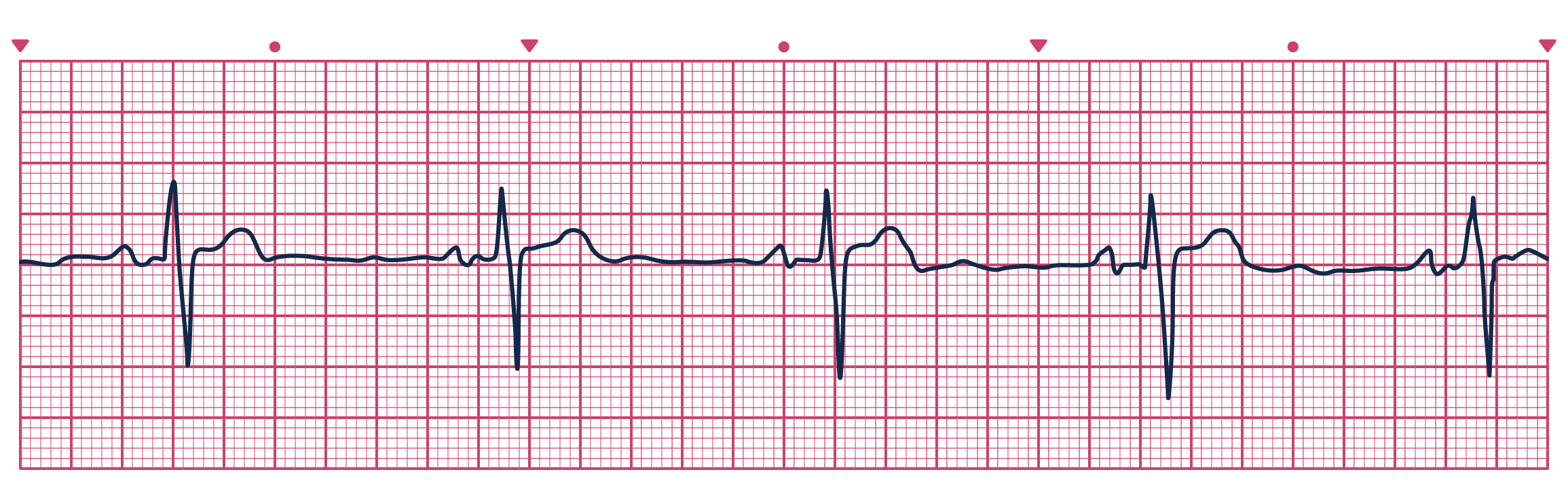
Idioventricular Rhythms
Indicate a dying heart with slowing rates. Common fatal rhythm in elderly patients. SA and AV nodes completely fail to fire, and impulses arise from the ventricular tissues in an attempt to prevent cardiac standstill. Very distorted QRS in every beat and no P wave. Idioventricular rates can be accelerated (> 100 bpm) or agonal (< 20 bpm).
Treatment: Atropine; pacing; dopamine or norepinephrine if hypotensive; imminent need for CPR and ACLS protocol!
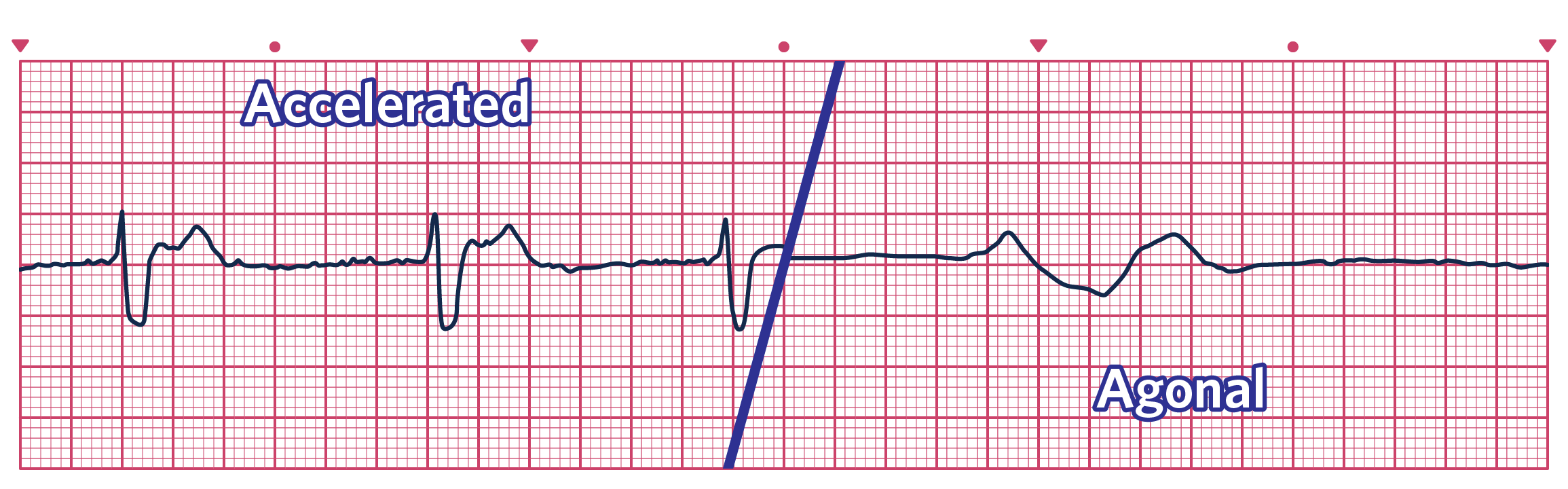
Five steps to identify this heart rhythm:
- What is the rate? Ventricular: > 100 bpm; typical 20-40 bpm
- What is the rhythm? Usually regular
- Is there a P wave before each QRS? Are P waves upright and uniform? Absent
- What is the length of the PR interval? Not measureable
- Do all QRS complexes look alike? What is the length of the QRS complexes? Similar but distorted; wide and distorted (> 0.12 sec), with T wave deflection
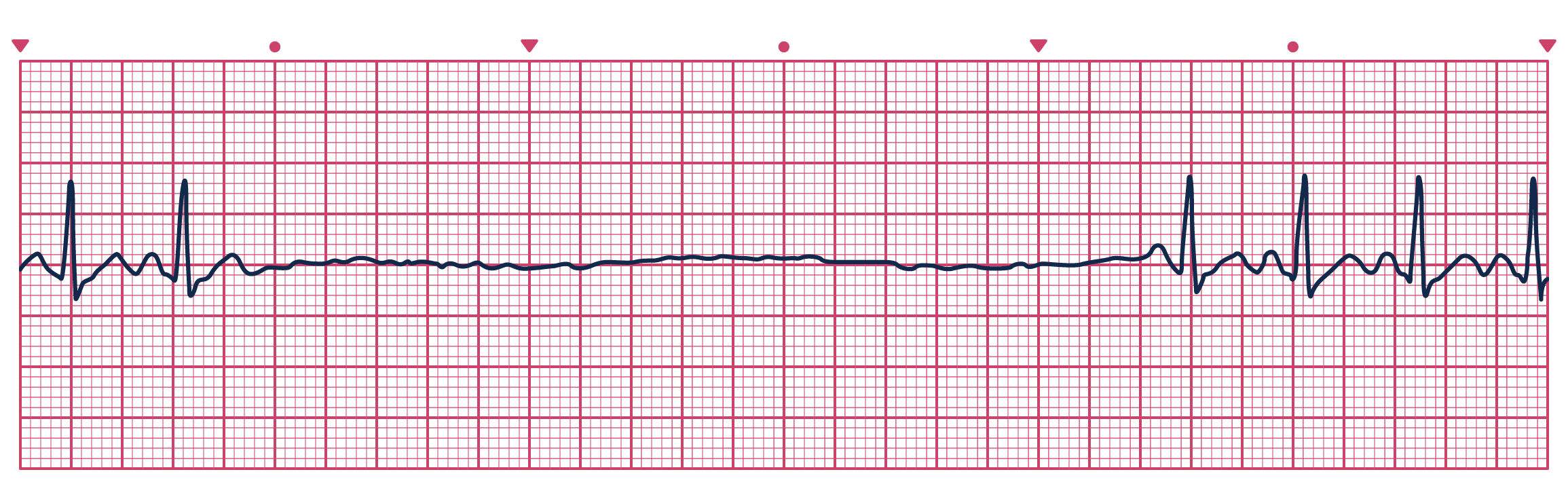
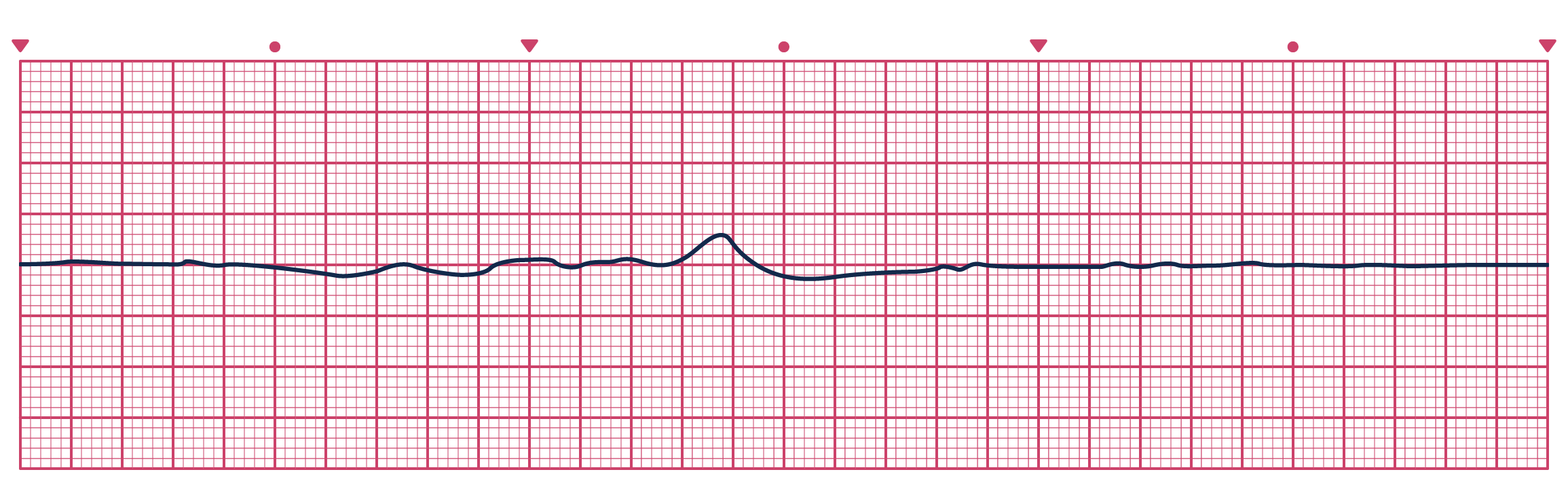
Asystole
Cardiac standstill. No deviation from the isoelectric line.
Treatment: Follow CPR and ACLS protocol.
Pulseless Electrical Activity (PEA)
The absence of a palpable pulse and myocardial muscle activity with the presence of organized electrical activity on the cardiac monitor. The patient is clinically dead despite some type of organized rhythm on monitor. This electrical activity can present in a variety of ways, but the key is that the heart has no mechanical activity.
Treatment: Follow CPR and ACLS protocol.